This month we focus on the cabinet reshuffle and implications for health and social care, the CMO’s annual report, a Q&A with the new Chair of the National Centre for Rural Health – Nigel Edwards, and other news including our Health and Care Seminar focusing on workforce issues on 29 November. Read on to find out more…
Cabinet reshuffle and health changes
It has been a month of big announcements in the world of politics. This week saw a major reshuffle in the cabinet with Victoria Atkins MP being named as the Secretary of State for Health & Social Care.
Ms Atkins has a background in law and order, practising as a criminal barrister specialising in serious organised crime. She was elected to the constituency of Louth & Horncastle in 2015 and in 2017 joined the Home Office. In 2021, she moved to the Ministry of Justice and then, in 2022, was appointed as the Financial Secretary to the Treasury. As a MP with a predominantly rural constituency, she says she fights for issues “including the provision of rural broadband, defence, wind turbines, coastal issues, roads, schools, the health service and the importance of the rural way of life.” On health issues, Ms Atkins has voted for reforming the NHS so GPs buy services on behalf of their patients.
Taking to Twitter following the announcement of her appointment she said: “Our NHS matters to us all, and I look forward to working with NHS and social care colleagues to bolster services during what promises to be a very challenging winter period, cut waiting lists and improve patient care.”
On her first day as Health & Social Care Secretary she met Professor Chris Whitty amongst others to discuss bolstering services for winter, cutting NHS waiting lists, improving patient care and ending industrial action. This is significant following Professor Whitty’s latest annual report Health in an Aging Society and the NCRHC hopes that Ms Atkins will work closely with him to address the issues he raised.
Other appointments as part of the reshuffle included Andrew Stephens MP as Minister of State in the Department of Health & Social Care. Also appointed to the department as Parliamentary Under Secretary of State, is Andrea Leadsom MP.
This month has also seen the King’s Speech in Parliament. Written by the government, this year it focused on growing the economy and law and order. The health-specific announcement included raising the age of sale for tobacco products, effectively eliminating smoking for the next generation.
It also mentioned the NHS Long Term Workforce Plan. King Charles said: “Working with NHS England my government will deliver its plans to cut waiting lists and transform the long-term workforce of the NHS.
“This will include delivering on the NHS Workforce Plan, the first long-term plan to train doctors and nurses the country needs and minimum service levels to prevent strikes undermining patient safety.”
However, there was a missed opportunity in this speech which has frustrated many health leaders. There was no mention of the mental health reform which is long overdue and means many people are living in a state of crisis with little or no access to services. However, with a General Election looming, one would expect this to feature as part of future electioneering.
Q&A with the new Chair of the National Centre for Rural Health & Care
This month, Nigel Edwards has taken over the Chair of the National Centre for Rural Health & Care. Nigel currently works as an associate with PPL Ltd, RAND Europe and the National Association of Primary care, as well as with the WHO on primary and hospital care in Europe.
He has been telling Casebook more about his work and what he hopes to achieve in his new role.
What is your professional experience of Rural Health & Care?
I have a long standing interest in hospital provision in rural and coast areas and have researched solutions and worked with people developing ideas to solve these problems. I have also done work on the challenges of rural primary care in the Republic of Georgia, Azerbaijan and Lithuania. Recently I have also been involved in helping to develop strategies for acute care in rural areas in Northern Ireland and Wales. As CEO of the Nuffield Trust I also encouraged my researchers to think about the rural dimensions of areas they were studying. The Trust has previously done work with the Centre.
What impact will the government’s Long-term NHS Workforce plan have on rural communities in its current format?
It is good that a workforce plan has been developed after a long wait and the general proposals to expand and strengthen the workforce are welcome and will benefit rural communities. However, the issues of rurality receive relatively little mention in the plan and there is more to do to develop specific responses to the particular problems of rural areas. The programme announced by HEE last year for rural and coastal areas is a good start but may need to be much more imaginative. New medical schools and local recruitment are a good start but perhaps we should also be thinking about whether we need professionals with a more generalist training and who are recruited to a different, more community oriented set of values than are often currently applied.
What one simple change can government make to improve the health and care for rural communities?
The easy answer to this is getting resource allocation right but, I have learned that in policy areas like this there are no single simple changes. This is a complex area and a range of complementary interventions designed to facilitate bottom-up change and based on a deep understanding of the issues is what is required. The coalition of interests around rural issues provides a great way of working out what needs to be done and how it can be achieved. That’s a good thing because unfortunately some of the policy machinery in central government has been weakened and will need all the help it can get.
Is there anything else you would like our Members to know?
I am very interested to hear from members about their ideas on how the Centre can help and their views on where there is an opportunity to make the most significant difference. You can contact Nigel here.
Rural Health and Care Seminar 29 November 2023
We’ve had over 120 bookings so far for the Rural Health & Care Seminar on Wednesday 29 November 2023. The free online event aims to discuss the topic of Rural Health and Care in England focusing on “Tackling the rural health and care workforce problem”. It will also consider in depth the points made in the National Centre for Rural Health and Care's paper in response to the NHS Workforce Plan.
Speakers include:
- Nigel Edwards, Chair of the National Centre for Rural Health and Care
- Professor Jim Rourke, Professor Emeritus & Former Dean of Medicine, Memorial University of Newfoundland, Canada
- Adrian Clements, Executive Medical Director, North Cumbria Integrated Care NHS Foundation
- Lisa Hughes, Associate Head of Workforce Transformation, Workforce Training and Education, NHS England
- Claire Flavell, Strategic Lead, Lincolnshire Talent Academy
If you haven’t already booked, please register here.
Chief Medical Officer’s Annual Report paints bleak picture for rural
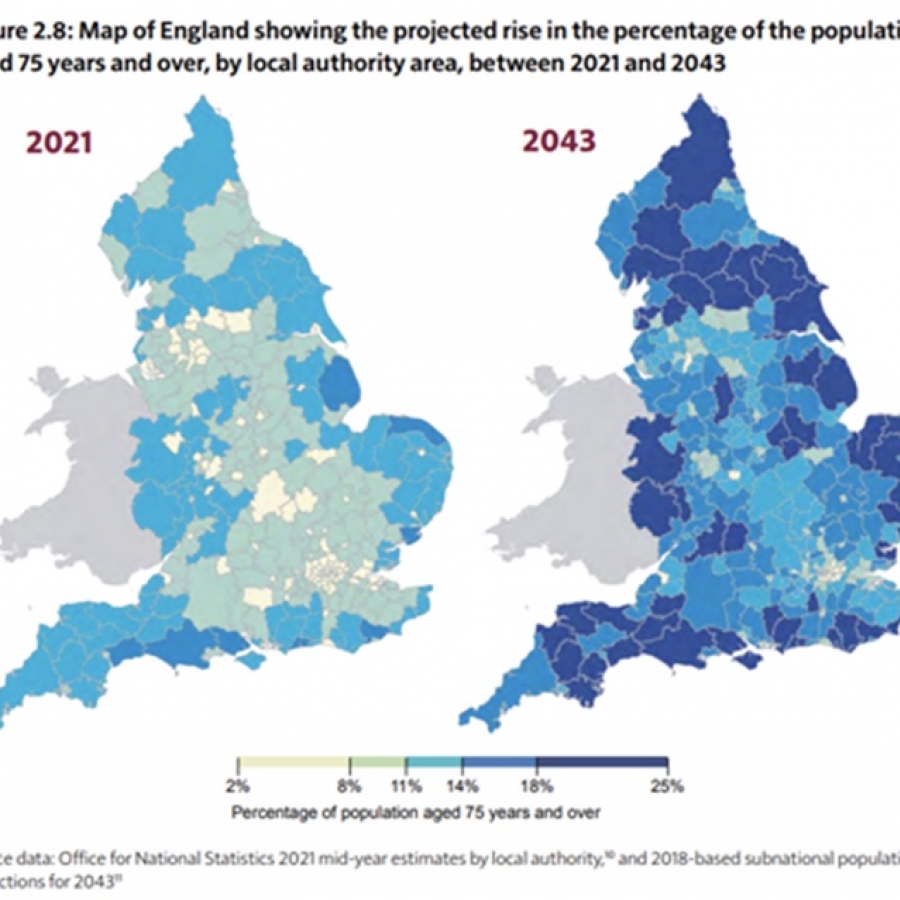
Last week the government’s Chief Medical Officer, Professor Chris Whitty, published his annual report, this year focussing on Health in an Ageing Society. In it, he says: “For policymakers, the biggest concern I have is that government and professional bodies have not recognised the degree to which the population living in older age is concentrating geographically in the United Kingdom in general, and England specifically. The great majority of people move out of cities and large towns before older age, concentrating geographically in coastal, semi-rural or peripheral areas, often with relatively sparse services and transport links.”
The report goes on to set out the challenges facing the aging rural population including the difficulty in recruiting staff in the social work and domiciliary care sector to look after these communities. It attributes these problems to high property prices in rural areas, poor public transport, high fuel costs and higher demands from the quantity of patients. The report warns that “if we do not tackle the health problems of these communities vigorously and systematically there will be a long tail of preventable ill health in peripheral areas which will get worse as current populations age.” This is supported by ONS figures which show a stark picture: