In this edition of Casebook we focus on the importance of digital connectivity in health and care provision in articles from BT and the Good Things Foundation; the benefits of local collaboration in designing health solutions; debate from the House of Lords on rural pharmacies; the growing need for rural supported housing; and an events update. Read on to find out more…
Telecare - Adjustment to digital switchover announced
BT Group has announced significant adjustments to its digital switchover programme, which aims to transition the UK's traditional analogue landlines to digital Voice over IP (VoIP) technology by January 2027. The revised approach will result in a single switch for most customers—from copper to fibre with all customers now expected to have moved off the old analogue PSTN by the end of January 2027.
This comprehensive switchover plan is part of a broader effort to prepare the country for a full-fibre future, aligning with the UK Government’s gigabit connectivity goals.
BT’s phased regional rollout plan for Digital Voice includes extensive awareness campaigns and local support to ensure customers understand the changes and are prepared for the switch. The transition to digital landlines is a pivotal step towards a fully connected, fibre-based future, supporting the UK’s broader gigabit connectivity ambitions.
For further information, read BT's official announcement in full.
This announcement delays the deadline for the switchover from 2025 to 2027.
Howard Watson, Chief Security and Networks Officer, BT Group, said:
“The urgency for switching customers onto digital services grows by the day because the 40-year-old analogue landline technology is increasingly fragile. Managing customer migrations from analogue to digital as quickly and smoothly as possible, while making the necessary provisions for those customers with additional needs, including telecare users, is critically important.
“Our priority remains doing this safely and the work we’re doing with our peers, local authorities, telecare providers and key Government organisations is key. But more needs to be done and we need all local authorities and telecare providers to share with us the phone lines where they know there’s a telecare user.”
For more information about the BT Voice Digital Switchover, please visit: https://www.bt.com/broadband/digital-voice
Kerry Booth, Chief Executive, Rural Services Network
"We are pleased that BT is delaying the switchover to digital lines to ensure that the most vulnerable are not left behind. This delay provides a crucial window for implementing the Shared Rural Network and improving the mobile network, which we anticipate will benefit rural communities significantly by then. Ensuring that all rural residents have reliable and efficient digital services is a priority, and we welcome BT's efforts to engage and support vulnerable communities throughout this transition."
The impact of local area coordination
The recent multi-site evaluation of Local Area Coordination (LAC) in England and Wales, funded by the National Institute for Health and Social Care Research and conducted in collaboration with leading universities, presents significant findings that underscore the transformative power of this approach. This research, published last week, is a landmark study, providing a comprehensive understanding of how LAC can make a meaningful difference in people’s lives and communities.
The study, undertaken by the Universities of Hull, Sheffield, York, Exeter, and Leeds, is the first of its kind to evaluate the LAC approach across multiple sites. It highlights the substantial benefits of LAC at individual, community, and systemic levels, showcasing its potential to revolutionise the way we think about and deliver preventive care.
Key Findings:
- Building Trust Through Relationships: One of the most crucial aspects of LAC is the emphasis on developing trusting relationships. Coordinators spend significant time with individuals, understanding their unique circumstances and building rapport. This trust is foundational to the success of LAC, enabling more effective support and engagement.
- Strengthening Community Connections: LAC works by connecting individuals to community resources and support networks. This approach not only reduces social isolation but also fosters a sense of belonging and community solidarity. The study found that these connections significantly enhance the overall wellbeing of individuals.
- Reducing the Need for Formal Care: By addressing issues early and providing continuous support, LAC reduces the reliance on formal care services. This preventive approach helps individuals manage their health and social needs more effectively, preventing crises and reducing the burden on formal care systems.
- Preventing Systemic Loss: Often times, individuals can get lost within the complexities of the health and social care systems. LAC ensures that people are guided through these systems, receiving the support they need without falling through the cracks. This role as a navigator is critical in maintaining continuous and effective care.
The research employed a Participatory Action Research approach, combining system and ward-level analysis, life stories, Qualitative Comparative Analysis, and a Nested Economic Study. These methods provided a holistic view of LAC’s impact and highlighted several critical aspects:
- Individual Impacts: Participants reported increased confidence, independence, and overall wellbeing. The consistent presence and support of Coordinators were pivotal in reducing stress and anxiety, enhancing individuals' capacity to cope with life's challenges.
- Community Impacts: The ripple effect of LAC’s community engagement was evident, with many individuals becoming more active in their communities. This engagement helped build stronger support networks and reduced social isolation.
- Systemic Impacts: LAC’s ability to bridge gaps in the public services system was a key finding. Coordinators effectively connected individuals with services and resources, reducing systemic barriers and promoting a more person-centred approach.
Local Area Coordination in Rural Communities
Rural communities face unique challenges, including limited access to transport, longer distances to medical facilities, an aging population, and healthcare workforce shortages. The findings from this study are particularly relevant to rural settings, where these challenges can significantly impede access to care.
LAC Coordinators act as connectors, ensuring that rural residents can access necessary services and support despite geographical barriers. By fostering local connections and support networks, LAC helps build resilient communities that can support their members more effectively. The emphasis on early intervention and continuous support aligns well with the needs of rural populations, where accessing timely care can often be difficult.
The multi-site evaluation of Local Area Coordination provides compelling evidence of its effectiveness in transforming lives and communities.
- Read the Summary Report Here.
- Read the Full Report Here.
Detailed in the Rural Access to Health and Care Services chapter of the Winning the Rural Vote Campaign, The Rural Services Network is committed to supporting such innovative approaches recognising their potential to address the unique challenges faced by rural and coastal areas. By investing in and expanding the LAC approach, we can make significant strides towards more equitable and effective health and care services for all.
Enhancing rural health access
It was recently Mental Health Awareness Week, during which the Rural Services Network shone a spotlight on the unique challenges faced by rural communities in accessing health and care services. These challenges, ranging from limited transport options to an aging demographic, significantly affect the mental and physical wellbeing of rural populations.
Rural residents often experience greater difficulties in accessing healthcare facilities due to longer travel distances and less frequent public transport services. This not only complicates emergency medical care but also the routine management of chronic conditions and mental health support. The aging population in rural areas, which is growing faster than in urban centres, further strains limited healthcare resources.
Funding Disparities
There is a notable disparity in funding between rural and urban areas, with urban local authorities receiving substantially more per capita for public health and social care services. This funding gap exacerbates the challenges of delivering care in rural regions, where costs are inherently higher due to the geographical spread of the population.
Innovations and Solutions
Addressing these challenges requires innovative solutions and a focus on local service provision. The Rural Services Network advocates for:
1. Enhanced Hospital Access: Improving transportation and accessibility for rural patients, visitors, and staff is essential. Expanding transport schemes could mitigate some of the current barriers to accessing healthcare.
2. Strengthening Local Care: Developing multi-disciplinary health hubs in rural towns can significantly reduce the need for long travel to hospitals. These hubs would provide a range of services locally, from routine check-ups to mental health support.
3. Boosting Public and Mental Health Services: Increasing resources for public and mental health services in rural areas is crucial. This includes addressing the funding disparities and promoting best practices that are tailored to the needs of rural populations.
4. Improving Social Care: Implementing fair funding models is necessary to meet the higher costs of delivering social care in rural areas. Enhancing engagement with local support services can also help in managing the complex health needs of the aging rural population.
5. Addressing Workforce Shortages: There is a critical need for a rural focus in the NHS Workforce Plan. Offering incentives for healthcare professionals to work in rural areas and incorporating rural placements in medical training could help alleviate some of the workforce challenges.
As we observe Mental Health Awareness Week, it is imperative to acknowledge and address the specific needs of rural communities in England. The commitment to improving rural access to health and care services not only supports the physical health of these populations but also their mental wellbeing, ensuring a holistic approach to healthcare that is inclusive of all geographic areas. By focusing on localised solutions and addressing funding disparities, we can build a more equitable healthcare system that truly caters to the needs of every resident.
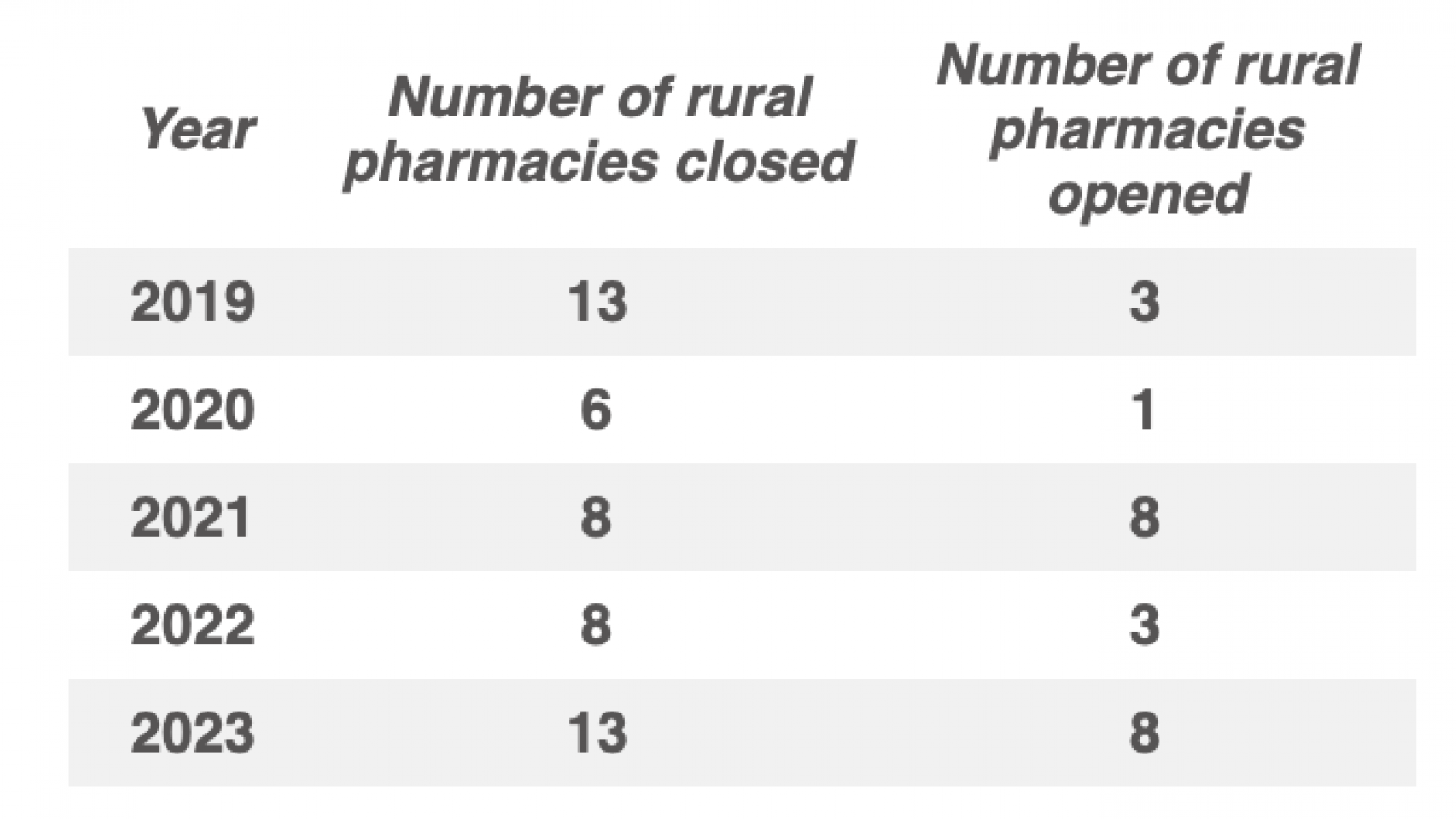
The impact of rural pharmacy closures
Rural communities in England are currently facing significant challenges due to the closures of community pharmacies, a vital resource for healthcare access in less densely populated areas. The recent peak in these closures prompts a critical evaluation of their impact on the health and welfare of rural populations.
In a recent session in the House of Lords, The Lord Bishop of St Albans inquired about the extent of these closures:
Question:
Lord Markham provided a detailed response illustrating the trend of closures over the past five years:
Answer:
"The below table shows the total number of community pharmacies that have closed and opened in rural areas in England, as defined by the Department for Environment, Food and Rural Affairs’ Guide to applying the Rural Urban Classification to data, each year from 2019 to 2023: