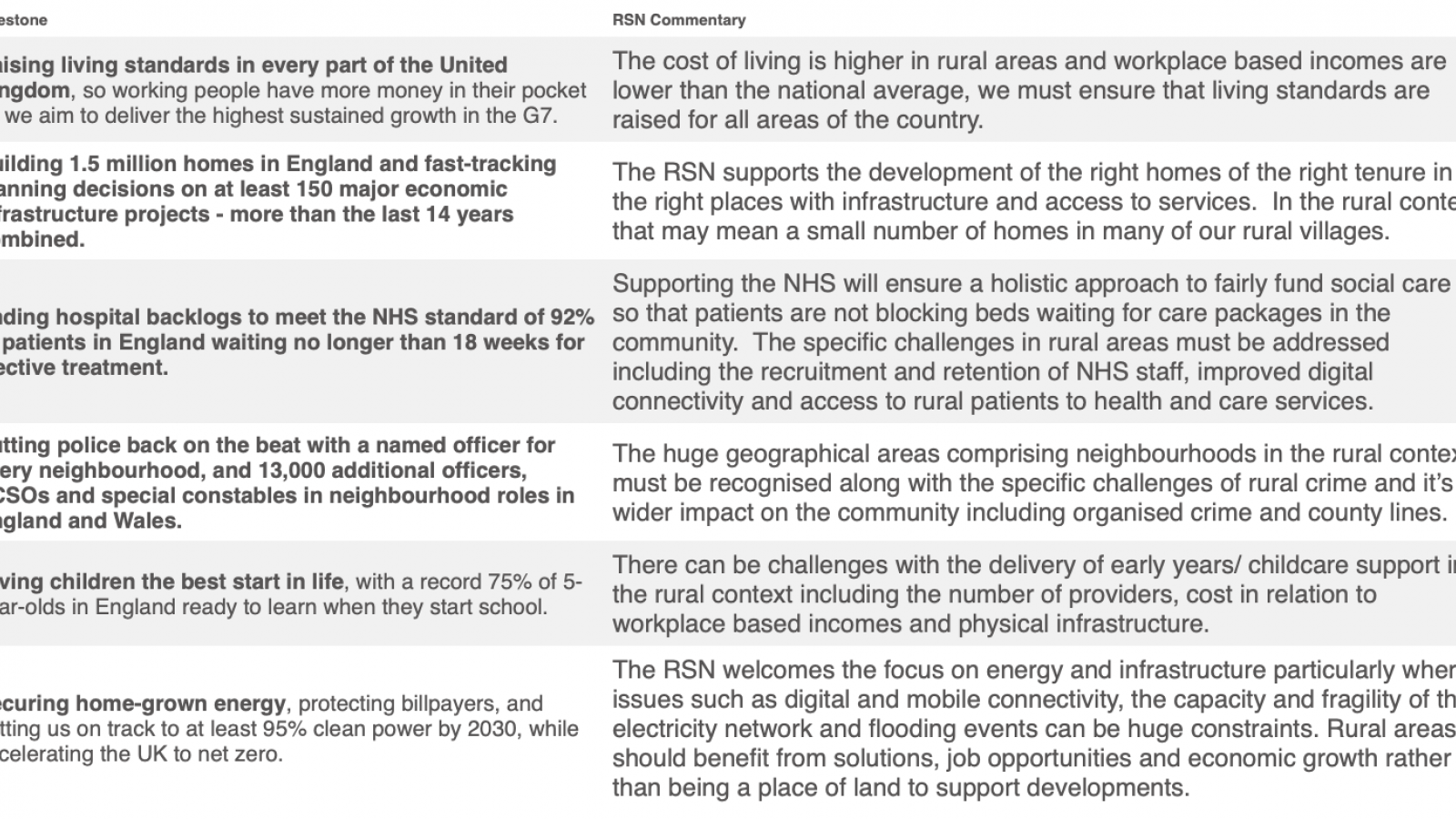
In short we welcome the Government’s approach to setting clear milestones for their missions, but we would like to see a focus on the challenges facing rural communities.
To hit these milestones, may require different policy solutions for rural areas to address any barriers to opportunity.
Pharmacies Vote to Cut Services in Protest Over Funding Shortfalls
Pharmacy owners across England, Wales, and Northern Ireland, including those in rural areas, have voted overwhelmingly to reduce opening hours and halt home delivery services in response to ongoing funding cuts. This historic move, orchestrated by the National Pharmacy Association (NPA), marks the first time pharmacists have taken such action in their history, highlighting the severity of the financial crisis gripping the sector.
The NPA represents approximately 6,500 community pharmacies, covering about half of the UK's total. A striking 99% of the pharmacy owners who participated in the vote expressed their willingness to limit services unless the government provides an additional £1.7 billion in funding. This call for extra support is particularly urgent for rural pharmacies, which often face unique challenges due to the higher costs associated with serving smaller, more dispersed populations.
Pharmacies in rural areas have long been a cornerstone of local healthcare, offering essential services that go far beyond dispensing prescriptions. These include home delivery services, advice on over-the-counter medications, and support for conditions such as diabetes, asthma, and high blood pressure. However, with core government funding for pharmacies in England having fallen by 40% since 2015 (after adjusting for inflation), many rural pharmacy owners are struggling to keep their doors open. Over the last two years, more than 700 independent pharmacies have shut in England alone—many of them in rural communities where access to healthcare services is already limited.
Rural pharmacies often face higher operating costs, including transportation to deliver medications to patients in isolated areas, and the challenge of attracting and retaining staff in locations where the cost of living may be lower, but so too is the local population. Despite these challenges, rural pharmacies are typically unable to raise their prices, unlike other businesses, as their funding is largely set by contracts with the NHS.
Pharmacy owner and NPA member, Ashely Cohen, explained that while 90% of their funding is fixed, costs for staffing, rent, and other overheads continue to rise, forcing many pharmacies to operate at a loss. “In rural areas, where patients depend on us for vital services, we simply can’t continue like this. Our goal has always been to support our communities, but we’re being squeezed to the point where we can no longer deliver,” Cohen said.
The NPA ballot, which saw a 64% turnout from 3,339 independent pharmacies, could lead to a range of service reductions. Among the proposed changes are limiting opening hours to no more than 40 hours per week, halting home deliveries of non-funded medications, and discontinuing services such as emergency contraception, smoking cessation programs, and support for substance misuse.
These cuts would severely impact rural patients, many of whom rely on their local pharmacy for convenience and essential health advice. For example, patients in rural areas may have limited or no access to other forms of healthcare, making pharmacies a vital resource. In rural communities, cutting services such as free monitored dose systems for the elderly and home delivery of medications could leave the most vulnerable without much-needed support.
Nick Kaye, Chairman of the NPA, emphasised the gravity of the situation, stating, “Rural pharmacies have been hit hard by years of underfunding. This vote is not taken lightly, but the reality is that we cannot continue operating under these conditions. If the government doesn’t act soon, rural communities will lose access to vital health services.”
The impact of pharmacy closures is not only felt by patients but also by the wider healthcare system. As the government pushes for a greater focus on community-based healthcare, rural pharmacies play an essential role in easing the pressure on hospitals and GP surgeries. Without adequate funding, this shift toward community care could be jeopardised, leading to more patients seeking hospital treatment for conditions that could have been managed locally.
Dr. Leyla Hannbeck, Chief Executive of the Independent Pharmacies Association, echoed these concerns, calling the current situation a “crisis” and urging the government to act before more rural pharmacies close their doors for good. "If pharmacies are forced to cut services or shut down, patients in rural communities will suffer the most,” Hannbeck said.
The Department of Health and Social Care has acknowledged the challenges facing community pharmacies, with a spokesperson highlighting the importance of these businesses in delivering healthcare in local communities. However, they also admitted that the current funding system is unsustainable and in need of urgent reform.
For now, the NPA is calling for immediate talks with the government to secure increased funding and avoid further closures. As the situation stands, rural pharmacies are at a crossroads, and without the necessary support, the very services that rural communities rely on could be in jeopardy.
Biggest Overhaul in a Generation for Children’s Social Care
The government is launching a major reform of the children’s social care system, described as the most significant in a generation. The aim is to address years of neglect and underinvestment, which have led to rising costs and poor care for vulnerable children. Spending on looked-after children has skyrocketed from £3.1 billion in 2009/10 to £7 billion in 2022/23, partly due to private care providers charging high fees while delivering subpar services.
Tackling Exploitative Care Providers
A key part of the reform is tackling private care providers that make excessive profits while failing to provide proper care. Ofsted will gain new powers to fine care providers that don’t meet standards, making it easier to crack down on unsafe homes. The government will also require large care providers to share financial information to ensure transparency and curb profiteering. If they don’t limit profits voluntarily, a new law will be introduced to cap them.
Focus on Early Intervention and Family-Cantered Care
The reform prioritises early intervention to keep families together and reduce the need for children to enter care. Families will have a legal right to be involved in decisions about their children's care, helping to prevent crises before they escalate. The government is also investing in preventative services to create a more sustainable care system.
Encouraging Not-for-Profit Providers
The government is encouraging not-for-profit providers and those backed by social investment to offer children’s care placements. This is aimed at reducing reliance on large private providers and ensuring that children are placed in safe, supportive environments.
The Rural Services Network’s Role
The Rural Services Network (RSN) will closely analyse how these reforms impact rural councils, where challenges such as lower population density and fewer resources can make delivering children’s services even more difficult. While the RSN welcomes these reforms as a necessary step forward for children’s social care, we recognise that rural councils will need additional support to effectively implement these changes.
The government’s focus on early intervention, financial transparency, and improving care standards is encouraging, but councils, particularly in rural areas, may face unique challenges in adapting to these new requirements. Rural councils often operate with smaller budgets and a more limited workforce, which can make it harder to introduce and manage these reforms. The RSN is committed to advocating for the resources and support that rural councils need to ensure these reforms are successfully implemented in all parts of the country.
Support from Key Figures
The reform has been welcomed by many experts, including Cllr Arooj Shah of the Local Government Association, who praised the focus on early intervention and tackling profiteering. However, she stressed that sufficient funding and resources are essential for success. Children’s Commissioner Dame Rachel de Souza emphasised the need for urgent reform to protect children from unsafe care and ensure they grow up in safe environments.
Looking Ahead
While the proposed reforms are a significant step forward, challenges remain, especially around funding and workforce capacity. The government will announce additional funding plans in the coming weeks, continuing the effort to transform the care system into one that prioritises children’s well-being.
Read the announcement in full HERE.
Unpacking the NHS Dental Recovery Plan with a Rural Perspective
The National Audit Office (NAO) has released an investigation into the NHS Dental Recovery Plan, pinpointing major challenges and progress in enhancing dental services in England, particularly underlining the acute struggles faced by rural areas. The investigation report emphasises the rural-urban disparities in service provision and the tailored responses needed to address these inequities.
The investigation highlights a dramatic decrease in accessibility to dental services, with rural areas particularly disadvantaged. The number of treatments provided through NHS dentistry dropped by 4.7 million in 2023-24 compared to 2019-20, and only 40% of the adult population in rural England had seen an NHS dentist in the 24 months up to March 2024, down from 49% before the pandemic. This decline is more pronounced in rural regions, where distances and travel times to the nearest dental clinics exacerbate accessibility issues.
Additionally, the financial commitment to primary care NHS dentistry has seen a real-term decline, impacting rural areas significantly due to their often-higher operational costs and lower patient density. The under-utilisation of dental budgets, with a reported £392 million underspend in the NHS dental budget in 2023-24, signals a missed opportunity for bolstering rural services, where such funds are desperately needed.
The NHS and the Department of Health & Social Care's £200 million Dental Recovery Plan aims to enhance access by adding over 1.5 million additional treatments by 2024-25. Key components such as mobile dental vans are particularly relevant for rural communities, aiming to mitigate the lack of fixed dental practices in these areas. However, the implementation has faced hurdles, including delays in deploying these mobile units, critical for extending reach in underserved areas.
Early indicators suggest that the plan is not meeting its intended goals, with significant implications for rural populations. As of October 2024, while some initiatives like new patient premiums and adjustments in UDAs have been rolled out, essential components like mobile dental vans have not been fully realised. This shortfall is troubling for rural areas, which benefit significantly from such flexible service delivery models.
The report calls for a comprehensive evaluation of what works, especially in the context of rural service delivery. There's a pressing need for the NHS and DHSC to refine their approach, considering the unique challenges faced by rural areas, such as geographic isolation, fewer healthcare resources, and higher operational costs. Improving engagement with Integrated Care Boards (ICBs) and local practices and ensuring that reforms address the specific needs of rural communities, are critical for making NHS dental services more equitable across England.
For those seeking a deeper understanding of the NHS Dental Recovery Plan’s impact on rural areas and its broader implications, the full report is accessible here.
Lee Summerfield, Report Director, summarises the findings in this video.
Latest Analysis of the Annual Population Survey Personal Well-being dataset
Through the answers given to four questions taken from the Annual Population Survey it is possible to gauge levels of life satisfaction, happiness, estimates of the feeling that things in life are worthwhile, and anxiety. This analysis presents this information against similar authorities to assist in monitoring local attitudes. Download the annual population survey personal well-being dataset analysis here
Latest Employment and Support Assessment Analysis
Employment and Support Assessment (ESA) is an income replacement benefit for people below state pension age. If someone has a health condition or disability, and for that reason are unable to work, ESA offers financial support and personalised help so that they can return to work if they are able to. The following analyses looks at the Employment and Support Assessment caseload as a proportion of total local authority population estimate, both for district and unitary authorities. The analysis shows the relative level of caseload and compares to key averages to provide a barometer of a local authority's particular situation.
- Download the ESA analysis (District) here
- Download the ESA analysis (Unitary) here
Free to attend Plymouth University Dementia Conference 11 April 2025
Once again, it’s that time of the year again for the International, National, Regional, and local Plymouth University Dementia Conference 2025. This year we have attracted interest from across the globe. From in person keynote speakers from China, Japan, Europe, Gibraltar, Belgium, Ukraine, Wales, and A.I. specialists talking about 12 innovative initiatives, there will be plenty of opportunities to network and share insights. The day promises to be both informative and engaging.
Please join us in person or online for this free to attend event with a silver lunch. This innovative and unique event will bring together inspirational speakers from around the globe to present their creative projects and research.
Chaired by Angela Rippon CBE and David Fitzgerald, the aim of the conference is to showcase the work of dementia awareness, dementia care research and the future of AI in the world of dementia support regionally, nationally, and internationally. We also wish to share thoughts and ideas which have the potential to open new ways of developing fresh perspectives and groundbreaking solutions that help overcome the challenges faced by people living with dementia and carers every day in their lives.
Below is the Website and registration link for the National and International Perspectives of Dementia conference at Home Park on April 11, 2025. Sign up early to avoid being disappointed (we have limited tickets)
https://www.plymouth.ac.uk/whats-on/national-and-international-perspectives-of-dementia